Patients living with breast cancer often encounter a lack of clear answers to the simplest questions about the interplay of treatment and lifestyle factors, such as nutrition, physical activity, and sexual health. Any advice that is available may be inconsistent and based on weak or even flawed data.
Speakers at the 2024 San Antonio Breast Cancer Symposium® reviewed relevant data, recommendations, and guidelines in these areas during Tuesday’s Special Session 3: Sex, Drugs, and Rock & Roll. The session recording will be available on demand for registered 2024 SABCS® participants through March 31, 2025.
Supplements and cannabis
Many breast cancer survivors seek a holistic approach that goes beyond just treating their disease, said Heather Greenlee, ND, PhD, MPH, a cancer epidemiologist and the Medical Director of the Integrative Medicine Program at the Fred Hutchinson Cancer Center.
This approach may include use of supplements or cannabis to mitigate adverse events associated with treatment. According to Dr. Greenlee, 50% to 85% of breast cancer survivors have reported using dietary supplements following diagnosis. However, even the most commonly used multivitamins and herbal supplements may be contraindicated due to antioxidant activity or estrogenic effects.
“Just because something is natural, does not mean it is safe,” she said.
Dr. Greenlee reviewed clinical practice guidelines authored by several organizations about dietary supplementation and breast cancer. Based on the available evidence, she said patients should avoid vitamin D deficiency, which can be easily monitored by a physician. Lavender aromatherapy has been shown to be beneficial for anxiety, and ginseng may be helpful for fatigue. Although cannabis is recommended for refractory chemotherapy-induced nausea and vomiting, Dr. Greenlee specified that data only weakly supports this recommendation.
“There is a whole host of other non-pharmacologic approaches that can be just as effective or more effective than dietary supplements,” she said. “The potential interaction with these [supplements] is incredibly high, and so pharmacy review is essential. We need to have informed decision making between patients and providers.”
An increasing number of cancer survivors are also using cannabis for pain, insomnia, mood, appetite, or just recreational use, Dr. Greenlee said. However, cannabinoid hyperemesis syndrome can exacerbate nausea and vomiting, as well as mood disorders.
“We really need to have an environment where physicians can have safe discussions with patients,” she said, noting that disclosure of cannabis use is low in general and even lower in areas where cannabis is illegal.
Exercise during treatment
Clearer evidence-based research supports the benefits of physical activity — “move more, sit less” — for both the general population and patients living with cancer, explained Rikki Cannioto, PhD, EdD, MS, Assistant Professor of Oncology in the Department of Cancer Prevention and Control at Roswell Park Comprehensive Cancer Center.
According to guidelines released by the Centers for Disease Control and Prevention in 2018, all adults, including those with chronic disease, should engage in a baseline amount of aerobic physical activity and strength training for major muscle groups.
In 2022, the American Society of Clinical Oncology recommended exercising while receiving cancer treatment to reduce fatigue, maintain physical function and strength, and enhance quality of life by reducing anxiety and depression.
“Despite these recommendations, a very small percentage of cancer survivors meet the physical activity guidelines for Americans. The prevalence is lowest in women and older patients,” Dr. Cannioto said. “Depending on the survey and depending on the age, approximately 40% to 60% of cancer survivors in the United States are entirely inactive, meaning no regular activity during their leisure time.”
To combat this issue, Dr. Cannioto analyzed data from over 6,100 patients across three studies, which, when pooled, found a 48.5% reduction in mortality for patients who self-reported meeting physical activity guidelines before, during, and/or after treatment, compared to those who were inactive.
This association remained true when looking at decreases in mortality by tumor subtype as well. There was also a 31% decrease in the risk of breast cancer recurrence among the physically active population.
“This is important because, to date, an association of post-diagnosis physical activity with breast cancer recurrence has not been well established in the literature, and there are actually few reports that look at specifically whether or not meeting the federal guideline for physical activity is associated with survival,” Dr. Cannioto said.
Eating and drinking
Lawrence Kushi, ScD, Director of Scientific Policy at the Kaiser Permanente Northern California Division of Research, discussed findings from the Pathways Study, a prospective study that evaluated the diets of women living with breast cancer based on a handful of previously established nutritionary guidelines. Healthier dietary patterns were associated with lower overall mortality and breast cancer-specific mortality rates, but dietary associations with breast cancer-specific mortality were less pronounced.
The Pathways Study also explored whether alcohol intake — a well-established risk factor for breast cancer — influences outcomes after breast cancer diagnosis as well. Dr. Kushi, the primary investigator for the study, said participants reported low overall alcohol intake — an average of about one drink per day — which may have influenced researchers’ ability to accurately determine associations.
“We don’t really see much of a relationship between the amount of alcohol people are reporting that they’ve consumed and the risk of recurrence, overall mortality, breast-cancer specific mortality, or cardiovascular disease mortality,” Dr. Kushi said.
Sexual health
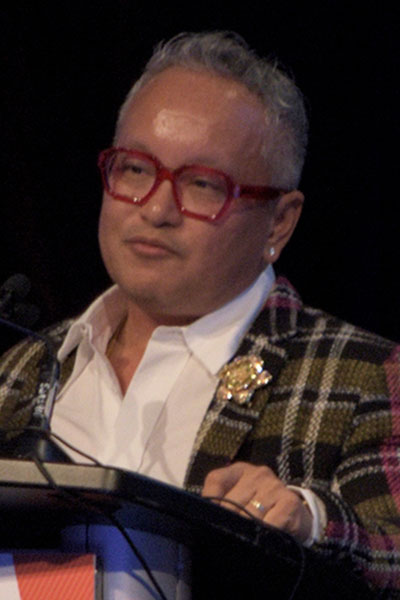
Don Dizon, MD, addressed sexual health after breast cancer diagnosis and emphasized that the incidence of sexual problems is significant regardless of whether a sexual organ is affected by cancer. Patients and their partners often suffer silently with this issue, said Dr. Dizon, the Founder and Director of the Oncology Sexual Health First Responders Clinic at Brown University Health.

“[Sexual health] is actually a complicated multidomain issue encompassing intimacy and sensuality, how one looks at themselves and their body image, arousal, desire, climax, and most of all, satisfaction,” Dr. Dizon said.
Dr. Dizon outlined treatments for overall sexual health, as well as vaginal health, including approaches for addressing genitourinary symptoms of menopause, sexual comfort, and sexual interest/arousal disorder.
Patient advocate Tomika Bryant, from King of Prussia, Pennsylvania, emphasized that a cancer diagnosis not only affects the body.
“It transforms our relationships, including our intimate relationships with ourselves and others,” she said. “Sexuality after cancer is often an unspoken journey, but one that deserves to be acknowledged and supported.”
Join us at SABCS 2025
Connect with thousands of basic and translational scientists, multidisciplinary clinicians, regulatory and pharmaceutical partners, survivors, and patient advocates at the 48th annual San Antonio Breast Cancer Symposium®. Complete your registration by Friday, September 26, to take advantage of discounted early registration rates.