Several supposed truisms exist in cancer drug development, from the idea that association with a poor prognosis makes a target ideal for study, to the assumption that there are simply too many mutations to ever fully untangle a specific cancer.
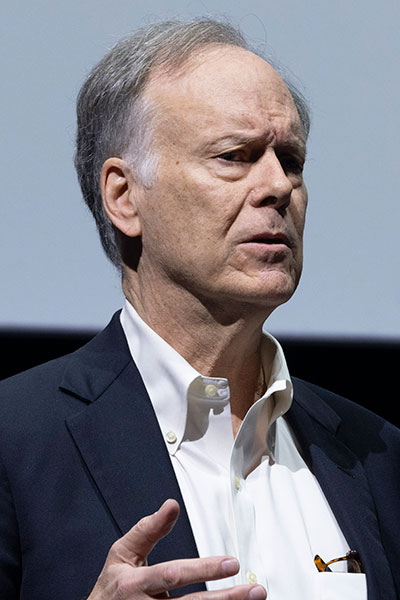
During a keynote address at the 2024 San Antonio Breast Cancer Symposium, Nobel Prize winner William G. Kaelin, Jr., MD, offered counterpoints from his work on the Von Hippel-Lindau (VHL) tumor suppressor protein, which helped lead to the successful clinical evaluation of vascular endothelial growth factor (VEGF) inhibitors and, more recently, the first hypoxia-inducible factor-2 (HIF-2) inhibitor to treat kidney cancer.
A recording of the address, delivered before General Session 1 on Wednesday, December 11, is available on demand for registered 2024 SABCS® participants through March 31, 2025, on the virtual meeting platform.
When considering new therapeutic targets, Dr. Kaelin said, it is important not to confuse correlation with causation when associating a specific biomarker with prognosis. He used the example of intratumoral hypoxia and the upregulation of the HIF transcription factor, which was historically associated with a poor prognosis.
“It’s certainly possible that hypoxia upregulates the HIF transcription factor and that HIF somehow causes aggressive tumor growth, but I would say that it’s even more likely that aggressive tumors outgrow their blood supply, become hypoxic, and thereby upregulate HIF,” he said.
Likewise, those biomarkers associated with a good prognosis should not be dismissed as focal points of study. Dr. Kaelin noted that estrogen receptor positivity is associated with a better prognosis than estrogen receptor negativity in breast cancer, but the role of estrogen has been a vital and valuable target in therapeutic research.
Once correlation and causality are separated, it is important to genetically validate targets and more fully understand their mechanisms of action.
“Having genetics on your side at least doubles your chance of success when you’re developing a new drug,” he said.
Genetic validation can be done in multiple forms, including studies that determine germline human variants or recurrent somatic mutations in particular cancers. Properly controlled somatic knockout or knockdown studies, using short hairpin RNAs or CRISPR, and mouse knockout studies also may be effective. Dr. Kaelin stressed that adoption of knockout or knockdown technologies without proper controls can lead to irreproducible findings or to findings that are not robust.
Dr. Kaelin drew another distinction when discussing the complexity of multiple driver mutations in a specific cancer, this time between necessity and sufficiency. He gave the example of a combination lock in which three steps are necessary to open the lock but undoing any one of those steps is sufficient to prevent the lock from opening.
“I actually think it’s a very good thing that most common cancers, including breast cancers, require multiple driver mutations,” he said. “I would even formalize this further and say that some of the mutations that occurred late during tumor evolution, whether they’re driver mutations or passenger mutations, are only tolerated because of the mutations that preceded them. If that’s the case, then correcting early mutations should selectively kill tumor cells.”
According to Dr. Kaelin, an additional reason to focus on early mutations is to help deal with intratumoral heterogeneity. With this, clonal events can lead to subclonal events, but Dr. Kaelin argued that a cancer therapeutic should be effective against all mutations rather than a small subset.
Dr. Kaelin also explored the concept of undruggable targets — another supposed truism in cancer drug development — through examples of his work with the VHL protein, which is mutated and inactivated in a large proportion of kidney cancers, and which, in turn, leads to upregulation of the HIF transcription factor.
“That’s the correlation, but someone had to do the work to establish that HIF was actually causal here,” he explained. “Many years ago, our lab showed that if you restored the function of the VHL protein in a VHL-defective renal carcinoma cell line, they lose the ability to form tumors.”
Subsequent complementary studies specifically focused on HIF, and the ability to form tumors was turned back on and then off again through manipulation of HIF isoforms. In combination with Dr. Kaelin’s lab’s target-credentialing studies on “the more famous member of the family,” HIF-1, they were eventually able to establish that it was HIF-2, not HIF-1, that led to cancer in VHL-defective cells.
“The 800-pound gorilla is clearly kidney cancers, where the VEGF levels go through the roof,” he said. “This makes sense because we know that an early event is loss of VHL, upregulation of HIF, and upregulation of VEGF. At that point, you probably remove the selection pressure to turn on other collateral alternative angiogenic factors.”
As HIF was historically deemed “undruggable” due to a lack of ligand-binding pockets, Dr. Kaelin returned to one of his guiding principles for drug development — “ignore the naysayers.” After further research, a druggable pocket of HIF-2 was found and exploited, eventually leading to the FDA approval of belzutifan.
In current drug development, Dr. Kaelin noted that there is an “explosion of interest” in developing small-molecule degraders for undruggable proteins. In addition, as the efficacy of targeted therapies increasingly comes into question due to inevitable resistance, Dr. Kaelin said, “the key is to combine multiple drugs against different targets … and you hope the toxicities don’t overlap in a prohibitive way, and you hope that they’re not cross-resistant.”
To build these novel effective combinations, Dr. Kaelin explained that specificity and potency will be important, and that the current mindset around using a maximum-tolerated dose of a single agent is probably antiquated in this context. Creative clinical trial design in the form of continuation of a drug after progression but in combination with a second drug also was proposed by Dr. Kaelin.
Dr. Kaelin was awarded the 2019 Nobel Prize in Physiology or Medicine for discoveries of how cells can sense and adapt to oxygen availability.
Access the 2024 SABCS® virtual platform
Watch any sessions you’ve missed and stay connected with fellow attendees in the online platform of the 2024 San Antonio Breast Cancer Symposium®. Recordings of sessions will be available on demand for registered 2024 SABCS® participants until March 31, 2025.

