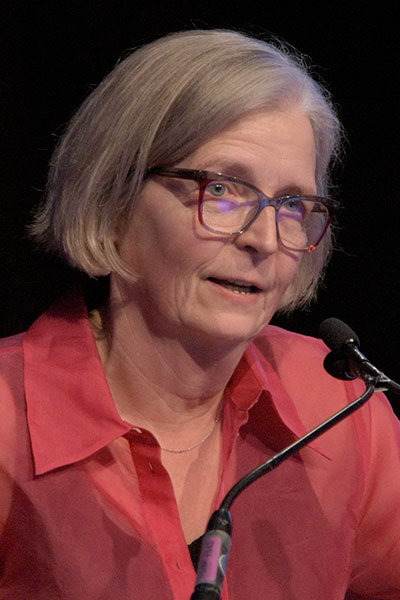
Steffi Oesterreich, PhD, recipient of the 2024 American Association for Cancer Research (AACR) Distinguished Lectureship in Breast Cancer Research, was recognized for her pioneering research investigating the role of estrogen receptor (ER)-positive tumor cells in resistance to endocrine therapy and for championing the concept that invasive lobular carcinoma (ILC) should be diagnosed and treated differently than other types of breast cancer.
She shared highlights from that seminal fundamental and translational research on ILC on Thursday, December 12, during the 2024 San Antonio Breast Cancer Symposium®. The session recording will be available on demand for registered 2024 SABCS® participants until March 31, 2025.
Dr. Oesterreich is the Shear Family Foundation Professor in the Department of Pharmacology and Chemical Biology at the University of Pittsburgh and Co-Leader of the Cancer Biology Program at UPMC Hillman Cancer Center. She also serves as the Co-Director and Director of Education at the Women’s Cancer Research Center, a collaboration between UPMC Hillman Cancer Center and the Magee-Womens Research Institute. The annual AACR Distinguished Lectureship in Breast Cancer Research, supported by Aflac, Inc., honors outstanding science that has inspired, or has the potential to inspire, new perspectives on the etiology, diagnosis, treatment, or prevention of breast cancer.
In her presentation, Invasive Lobular Breast Carcinoma — Old Idea, New Attention, Dr. Oesterreich credited her early work on ER cofactors for leading her toward research on ILC. The expression of some ER cofactors is high in ILC, which accounts for 10% to 15% of all breast cancers and mostly expresses ER.
The diagnosis of ILC is based primarily on histology and is characterized by loss of E-cadherin and the infiltrative growth of dyscohesive cells. ILC is the second most common histological subtype of breast cancer and the most common special histological subtype of breast carcinoma. The incidence of ILC has been increasing in recent decades.
Meta-analyses conducted by Dr. Oesterreich and her collaborators, which were presented at the 2021 SABCS®, showed no difference between the efficacies of aromatase inhibitors and tamoxifen, a selective estrogen receptor modulator (SERM), in ILC compared with the more common invasive ductal carcinoma.
“But we also realized that there was large discordance in ILC diagnosis [in the three studies included in this meta-analysis] and overall, there were worse outcomes for patients with ILC,” she said.
Realizing the need for biomarkers that predict response to hormonal treatments in patients with ILC, Dr. Oesterreich and colleagues have initiated a preoperative window trial to assess response to different endocrine therapies — fulvestrant, tamoxifen, and anastrozole — in patients with ER-positive human epidermal growth factor 2 (HER2)-negative post-menopausal women diagnosed with ILC.
To gain further insights into the poor prognosis of patients with ILC, Dr. Oesterreich and colleagues analyzed data from over 33,000 patients with breast cancer who were treated at one of three institutions within the Great Lakes Breast Cancer consortium. In this cohort, which included over 3,600 patients with ILC, patients with ILC experienced worse disease-free survival and overall survival. These findings were confirmed in a more recent collaborative study that included patients from four different clinical trials.
“What options are there for therapy in ILC?” Dr. Oesterreich asked, noting that the goal is to have precision oncology approaches that can benefit patients diagnosed with ILC. She reviewed recent collaborative research characterizing the profile of the tumor immune microenvironment and growth factor receptor pathway features, such as higher rates of PTEN inactivating alterations and enrichment of HER2 mutations, which may inform the development of targeted therapies for ILC.
Dr. Oesterreich reviewed some unique aspects of ILC research, including the development and credentialing of cellular models for ILC and the generation of ILC patient-derived organoids. The goal of these ongoing efforts is to develop validated models of ILC that can be a resource for the broader breast cancer research community. Additionally, her group developed models of ILC metastases that recapitulate the biological behavior of ILC, such as the propensity for leptomeningeal metastasis.
Dr. Oesterreich also spearheaded annual ILC meetings for researchers, clinicians, and patient advocates. At the first of these meetings, held in 2016, she met Leigh Pate, a patient advocate and founder of the Lobular Breast Cancer Alliance (LBCA). Since then, the LBCA, an organization formed by ILC advocates and researchers, has expanded partnerships with other organizations to fund ILC-focused research.
Dr. Oesterreich called attention to important active collaborations within “the relatively small field” of ILC, including studies led by the Great Lakes Breast Cancer ILC consortium. She highlighted LBC Monitor, a recently opened liquid biopsy trial in patients with metastatic ILC that is evaluating de-escalation of CDK4/6 inhibitor therapy in the first-line endocrine therapy setting.
Dr. Oesterreich also offered a look to the future and highlighted key research priorities in ILC. These include new diagnostic tools, imaging with novel tracers, models of ILC dormancy, the discovery of novel therapeutic targets, and insights into the lineage of disease.
She concluded by encouraging audience members to engage with the many ILC-related presentations at the 2024 SABCS®, including Poster Spotlight Session 18: Advancing our understanding of invasive lobular carcinoma: Potential to develop personalized therapeutic strategies? and more than 50 other posters on ILC.
“There is clear increased awareness and interest of ILC as an independent breast cancer subtype by clinicians, researchers, and patients,” she said.
Access the 2024 SABCS® virtual platform
Watch any sessions you’ve missed and stay connected with fellow attendees in the online platform of the 2024 San Antonio Breast Cancer Symposium®. Recordings of sessions will be available on demand for registered 2024 SABCS® participants until March 31, 2025.

